Okay here we go:
- malocclusion: basically an occlusion is a correct bite so malocclusion is a bad bite. easy!
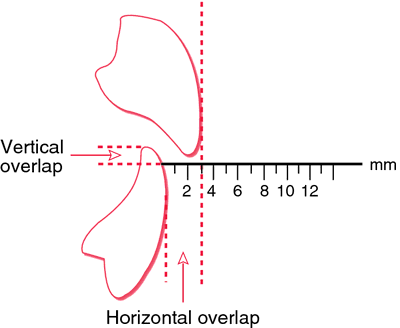
- class II malocclusion: this is an overbite, when the top jaw is vertically over your bottom jaw. There's also something called overjet which is a horizontal overlap. These kind of confused me for a while, but now I get it. An overbite is a deep bite, the bottom of the top teeth go down too low onto the lower teeth. The overjet is just having them too far ahead of the lower teeth.
 |
| http://medical-dictionary.thefreedictionary.com/overjet |
- class III malocclusion: this is an underbite, lower jaw in front of top jaw. This is me!
- class I occlusion: beautiful! perfect bite, everything is where it should be :)
- osteotomy: a surgery in which a bone is cut. It can be to lengthen, shorten, or change an alignment.
- the prefix osteo=bone
- Le Fort osteotomy: this is an osteotomy of the facial bones. There are 3 different procedures that I'm familiar with. Each of them break the bone in different parts of the face. I'm getting a le fort I (the one on the left).
- Le Fort 1 osteotomy: basically they break the bone a little bit above the base of the nose so that they can reposition the top jaw. Most incisions are done through the mouth cavity so there are little to no scars. It can impact the shape of the nose, upper lip, and of course, the upper jaw. It can be used to fix a gummy smile, an underbite, sleep apnea (by opening the airways), an overbite, and a cant in the jaw (a tilt). If the jaw is pushed forward, the nose typically widens and nostrils can looked flared due to the tip of the nose being pushed upwards. There are maneuvers and special stitches that surgeons can use to try to prevent these changes (VY stitch, alar base cinch suture, projecting the jaw in a certain direction up/down). The soft tissue changes after a le fort 1 are moderately unpredictable and vary from person to person. Sometimes the upper lip can collapse and recede, but I'm hoping that doesn't happen to me! There is less chance of nerve damage with just the le fort 1 procedure when compared to a BSSO.
- I'll find some more detailed photos later
- I'm sorry, I don't know a lot about the other 2 le fort procedures.

- orthognathic: can't believe I forgot to mention this one first. This is the type of surgery I'll be having. orthognathic comes from the greek words ortho meaning straight and gnathic meaning jaws. so literally: straight jaws! and who doesn't want that?!
- just to mention, my surgeon is an oral and maxillofacial surgeon and is certified by AAOMS as most doctors should be if they perform this type of surgery.
- BSSO: bilateral sagittal split osteotomy
- well we already learned osteotomy= bone break so that's easy
- bilateral: both sides of the jaw
- sagittal split: sagittal refers to the place on the mandible where the split is made
- this is not the procedure I am having as long as my le fort 1 is sufficient. If I were to have it, it would be cut and brought back. This can be used to correct an underbite, overbite, sleep apnea (by opening the airways), and a cant in the jaw. There's more risk of nerve damage as there's a nerve that will be screwed into if internal rigid fixation is used. The alternative to risking that damage is to have the patient remain wired tightly shut to support that jaw until the bone has had sufficient time to heal. (at least 6 weeks eek!) My surgeon really didn't want to risk the nerve damage.
- The nerves at risk are sensory nerves so a patient who loses feeling in these nerves will not appear to be a stroke victim. They just may dribble on their chin and not feel it or chew their lip and not feel it; things like that. The chances of not regaining full feeling back into that area is high enough to be negligible (I want to say 20%, but look it up!!) and increases with age. Full feeling is said to return between 6 months to a year after surgery and what the patient is left with after about a year is likely to be permanent and has a name starting with a p... paresthesia?
- There are also variations on this BSSO, there's bilateral sagittal split ramus osteotomy and a few others I've come across, but I'm not sure of what they entail because my research has centered on the le fort 1 procedure
- maxilla: this is the upper jaw
- mandible: lower jaw
I just found this site that has some good information, visuals, and case studies:
http://www.drclauser.com/pages/en/cranio-maxillo-facial-surgery-orbital-eyelids-surgery-reconstructive-aesthetic-surgery-oral-surgery-implantology/dento-facial-deformities.php
Leave me a comment if you're confused about something and I'll try to update when I think of other terms that might be helpful.
disclaimer: I really want to stress that this was all written by me, an untrained college student who has scoured the internet, medical journals and case studies, and asked my doctors for all of this information. I have no training in maxillofacial surgery so please don't quote me on any of this as it could be wrong.
However, it is factual to the best of my knowledge :)
No comments:
Post a Comment